A new trend has emerged among individuals aiming to lose weight: microdosing the diabetes medication Ozempic. As obesity and overweight rates soar, particularly in the United States, people increasingly turn to weight-loss drugs for help. Despite being approved for type 2 diabetes, Ozempic, alongside Wegovy, finds off-label use for weight management.
- Microdosing Trend: Some individuals use smaller-than-prescribed doses of Ozempic to manage weight, despite its primary approval for type 2 diabetes and lack of FDA endorsement for this practice.
- Motivations Behind Microdosing: Cost reduction, fewer side effects, and medication supply shortages drive this trend, though it compromises proven safety and efficacy standards.
- Risks and Concerns: Experts warn that microdosing can lead to suboptimal weight loss, uncontrolled diabetes, and risks from unregulated compounded medications.
- Holistic Approach Needed: Sustainable weight management requires combining medication with lifestyle changes, including exercise and diet modifications, to ensure long-term benefits.
Dr. Alexandra Sowa, an obesity medicine specialist, explains that microdosing involves using smaller doses than those typically prescribed. This practice, however, lacks approval from the U.S. Food and Drug Administration (FDA). Health professionals generally advise against it, as standard dosages derive from clinical trials determining safety and effectiveness, according to Shiv Sudhakar of the New York Post.
Ozempic contains semaglutide, a medication initially developed to manage blood sugar levels in type 2 diabetes patients. Its effectiveness in appetite suppression and weight loss stems from its ability to mimic the GLP-1 hormone, which slows gastric emptying and increases feelings of fullness. However, these benefits require careful dosing based on clinical trials. Off-label microdosing bypasses this evidence, posing risks that underline the need for professional guidance.
Dr. Fatima Cody Stanford, from Massachusetts General Hospital, notes that microdosing often stems from misconceptions about starting doses or gradual dose escalation. Many people attempt microdosing to reduce costs. With Ozempic’s average monthly retail price exceeding $1,000 without insurance, people see microdosing as a way to stretch their medication supply.
Reducing side effects forms another motivation for microdosing. Some individuals hope smaller doses will mitigate nausea, vomiting, or stomach discomfort. However, experts warn that lower doses may diminish the medication’s effectiveness proportionally.
Supply challenges also contribute to microdosing’s popularity. Dr. Amy Rothberg from the University of Michigan highlights that individuals may perceive benefits, even if they are minimal, due to the placebo effect. Nonetheless, the primary risk remains a lack of effectiveness since microdosing is unproven and unsupported by clinical studies.
The rise in obesity rates and the prohibitive cost of weight-loss medications like Ozempic highlight systemic issues in healthcare affordability and accessibility. Despite its popularity, microdosing reflects a deeper challenge in addressing chronic health issues through long-term strategies rather than quick fixes. Healthcare systems must balance innovation with affordability to ensure equitable access to effective treatments.
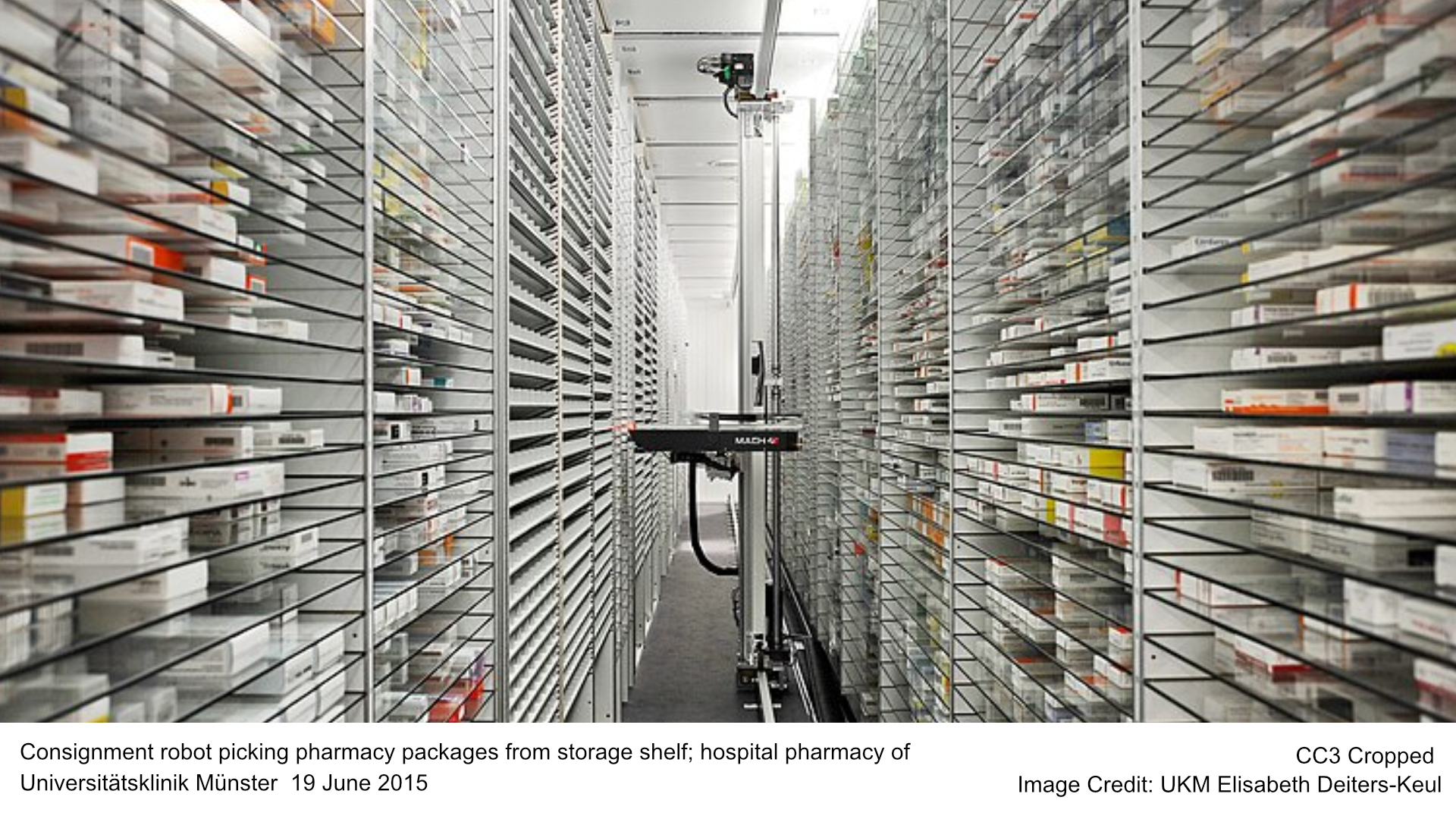
Dr. Stanford stresses that inadequate dosages can lead to uncontrolled diabetes and associated complications, as well as suboptimal weight loss. Additionally, compounded medications, often used in microdosing, lack FDA regulation, posing risks like contamination and inconsistent formulations.
Despite these concerns, some healthcare providers consider microdosing for select patients under close supervision. Dr. Suzanne A. Trott, a plastic and general surgeon, argues that, with proper monitoring, microdosing presents minimal risk. However, experts agree on the necessity of consulting healthcare professionals before altering medication regimens.
Sustained weight loss, experts emphasize, requires more than medication. Dr. Rothberg cautions against relying solely on drugs, advocating for lifestyle changes alongside treatment. Without such changes, the long-term benefits of medication will dwindle once stopped.
Dr. Trott recommends maintaining exercise, strength training, and a high-protein diet to preserve muscle mass. While microdosing remains a contentious subject, it underscores the growing demand for affordable weight-loss solutions.



Be First to Comment